INTRODUCTION:
The use of Peripherally Inserted Central Catheters (PICCs) has increased significantly in the last years due to their advantages compared to the other types of central catheters: easier and protocolized insertion by specialized nurse-led teams; cost-effectiveness; ease of management, ... However, an increase in the incidence of Catheter Related Thrombosis (CRT) has been observed with this type of device, especially in cancer patients and in the critical care setting. The main objective of this study is to determine the incidence of PICC related deep venous thrombosis in oncologic and onco-hematologic patients at the Donostia University Hospital, in Spain. The secondary outcome is the identification of possible risk factors associated with this event.
METHODS:
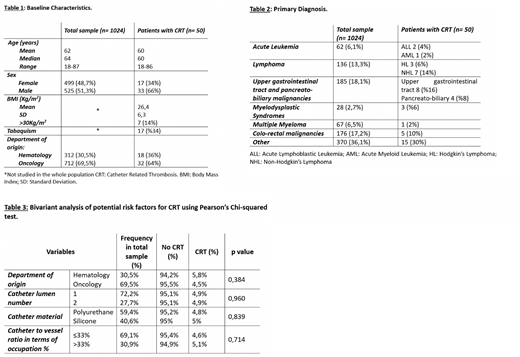
Using the database created and handled by the nurse-led Intravenous Therapy Team (ITT) in our center, in which all inserted PICCs are prospectively and consecutively included since 2011, a retrospective analysis was conducted on oncology and hemato-oncology-derived adult patients (over 18 years old) with a PICC inserted between May 15th 2018 and December 15th 2019. In the total population, several characteristics of the patient, of the PICC and of the thrombotic event were descriptively analyzed, and a bivariant analysis of four potential risk factors was carried out using Pearson's Chi-squared test. Patient and CRT treatment-associated risk factors were more exhaustively analyzed in the subgroup of patients with CRT. The missing data were obtained from the electronic clinical history records.
RESULTS:
The final study sample consisted of 1024 PICCs (n=1024), 19,10% (n=313) derived from the Hematology department and 43,62% (n=715) from the Oncology department (tables 1 and 2). The global incidence of CRT was 4,9% (n=50): 5.8% in hematologic patients and 4.5% in patients derived from Oncology. In the bivariant analysis no significant association was found between the selected potential risk factors (department of origin, PICC lumen number, PICC material and the catheter-to-vessel ratio) and CRT (table 3). In terms of the treatment administered to patients presenting CRT, in 80% of the cases (n=40) a Low Molecular Weight Heparin (LMWH) at therapeutic dose was initiated; in 10% (n=5) LMWH at a lower dose, and in 2 patients treatment could not be initiated because of thrombopenia. Finally, the PICC was withdrawn in only 8 patients after the diagnosis of the thrombotic event.
CONCLUSIONS:
The majority of the studies on PICC associated venous thrombosis in cancer patients are small, observational, retrospective, and without comparison groups. Here we present a work with an important sample size, a homogeneous population and with a prospective data collection. The CRT incidence has been similar to that described in the literature and significant association has not been found between the included potential risk factors and CRT. In conclusion, this study reflects the need of more trials on this subject, in particular to identify CRT risk factors in order to design effective prevention strategies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal